MACRA, MIPS and APMs
Download our helpful visual guide to understand your payment model options!
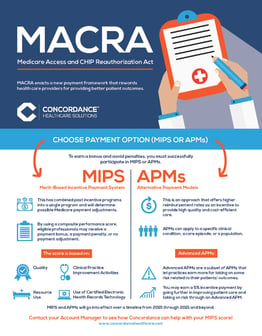 The Medicare Access and CHIP Reauthorization ACT (MACRA) enacts a new payment framework, the Quality Payment Program (QPP), that rewards healthcare providers for providing better patient outcomes. This visual guide explains the two pathways for determining payment adjustments to eligible providers:
The Medicare Access and CHIP Reauthorization ACT (MACRA) enacts a new payment framework, the Quality Payment Program (QPP), that rewards healthcare providers for providing better patient outcomes. This visual guide explains the two pathways for determining payment adjustments to eligible providers:
- Merit-based Incentive Payment System, or “MIPS”
- Alternative Payment Model, “APMs”
Concordance is dedicated to helping primary care providers make the transition from the current fee for service model to the quality based model in an easy and efficient manner.
Learn more about our visual guide by completing the form.




